This market resolves YES if a large insurance company covers more than 50% of a weight loss drug (e.g. Ozempic) for weight loss. This market resolves NO if that does not happen.
A large insurance company is one of the ten on the following list:
UnitedHealth Group
Kaiser Foundation
Elevance Health (formerly Anthem)
Centene
Humana
CVS Health
HCSC
Cigna
Molina Healthcare
Independence Health Group
For weight loss means that some non-diabetics are receiving coverage for the drug to loss weight.
People are also trading
I can confirm that they are already covered by major insurance plans, but the premise of this question is somewhat flawed.
Large insurance companies are offering plans that cover drugs as specified in your criteria, and have been doing so for some time already. However, each company offers multiple plans under their brand, which may have different formularies and copay/coinsurance percentages. The different plans can also be contracted with different PBMs. In short, it is possible for the criteria to be met and not met at the same time. Coverage can also depend on the network of the providing pharmacy.
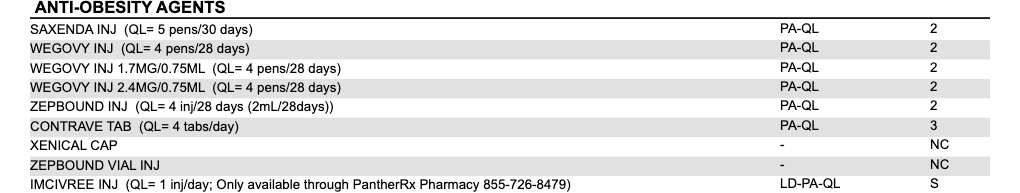
Anyway, if you needed proof to resolve yes, here is my plan's formulary (Anthem). Tier 2 is a $30 copay for 30 days, or $60 for 90 days in network, 50% OON. Tier 3 is $50 and $100. NC is not covered. S is specialty, 30% with a cap of $150